Brain Injuries: Symptoms and Treatments
What are brain injuries in children?
Also called pediatric traumatic brain injuries (TBI), traumatic brain injury is a broad term describing a range of symptoms that can be mild, moderate, or severe. TBIs result from a direct or indirect blow to the head. They can include:
Can a child recover from a TBI?
The degree of recovery from a TBI depends on the severity of the injury. Most children recover with no long term problems. However, more severe TBIs can cause lasting damage.
The severity of a TBI is determined by many factors including:
Symptoms can vary depending on the site of injury, extent of damage to the brain, and the child’s age or stage of development. Because a child’s brain is still developing, TBI in children is a chronic disease process rather than a one-time event; symptoms may change or become noticeable over time.
What are the types of TBIs?
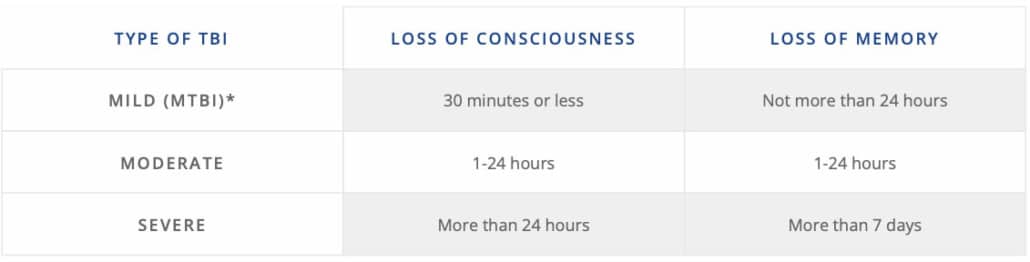
TBIs are defined as mild, moderate or severe based on the duration of loss of consciousness and/or memory loss.
| Type of TBI | Loss of consciousness | Loss of memory |
|---|---|---|
| Mild (mTBI)* | 30 minutes or less | Not more than 24 hours |
| Moderate | 1-24 hours | 1-24 hours |
| Severe | More than 24 hours | More than 7 days |
*Most concussions are mTBIs.
What are symptoms of a TBI?
Regardless of the type of TBI, signs and symptoms may be similar; however, in moderate and severe TBIs, symptoms may be more critical or acute. Symptoms can get worse over time and last weeks, months or longer.
Common signs of a TBI include:
More severe symptoms in a small percentage of children with a TBI include a long loss of consciousness, spasticity, muscle weakness, seizures, and more severe brain and functional problems.
How are TBIs in children diagnosed?
If your child has had a head injury or shows signs of a TBI, schedule an appointment with their primary care provider (PCP) or pediatrician. The provider will ask for details of the injury and symptoms and may do a physical and neurological evaluation to assess your child’s:
Depending on the results of this evaluation, your child’s medical provider may order an MRI or CT scan.
How are TBIs in children treated?
Your child’s treatment plan will depend on the severity of the TBI as well as your child’s symptoms, age, developmental stage and more. Rest will be recommended to support your child’s brain and body. An individualized treatment plan will be created in partnership with you with the goal of getting your child back to normal activities.
Your child’s treatment plan may include the following medical specialties:
In extremely rare cases, surgery may also be recommended as part of a child’s treatment plan.
DMG CRS includes all the medical specialties and support services to enable your child to receive coordinated care for their TBI in one, easy to access, child-friendly location. With your child’s entire medical team in one location, a single medical record accessed by all your child’s physicians, and on-site support services including labs, imaging, a pharmacy, social workers, and more, you can feel confident that your child will receive individualized, compassionate, coordinated care. Our goal is to enable you to focus on the health and wellbeing of your child and family throughout the treatment journey.